Department: Pediatric Orthopedic
Patient: male, age: 13Y
Dr. Danny Weigl, Head of the Pediatric Orthopedic Unit at Schneider Children’s Medical Center
Dr. Paz Kedem, Pediatric Orthopedic Surgeon
Dr. Eli Sidon, Pediatric Orthopedic Surgeon
Services: Segmentation, surgery planning, anatomy model
Background on the Condition: Slipped Capital Femoral Epiphysis (SCFE)
Slipped Capital Femoral Epiphysis (SCFE) is an orthopedic pathology in which the femoral head slips posteriorly relative to the femoral neck due to weakness in the growth plate. This condition is common among adolescents and, if left untreated, can lead to pain, restricted mobility, and progressive joint dysfunction. One of the main challenges in SCFE correction is maintaining the anatomical alignment of the femoral head while minimizing damage to blood vessels and soft tissues.
Institutional Background: Schneider Children’s Medical Center
Schneider Children’s Medical Center is a leading pediatric hospital in Israel, providing advanced medical services to children and adolescents. The hospital’s Pediatric Orthopedic Unit specializes in treating complex conditions such as SCFE, utilizing innovative technologies to improve clinical outcomes.
Surgical Planning and Execution Using 3D Printing Technologies
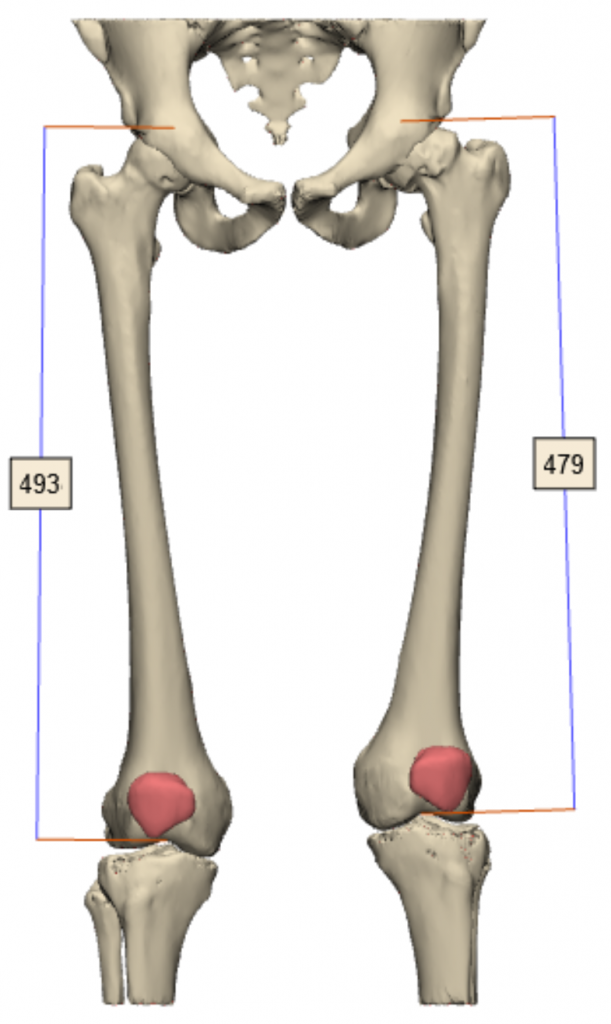
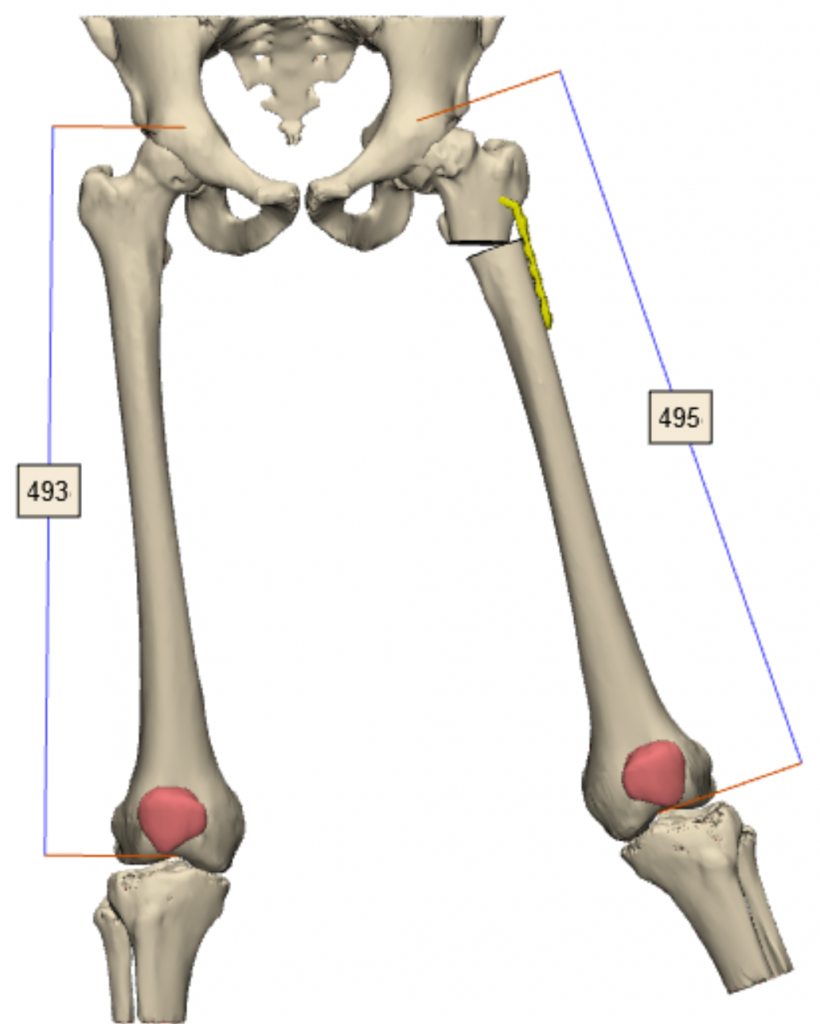
3D Planning Based on CT Imaging
Advanced 3D imaging of the patient’s unique anatomy was performed based on CT scans, in collaboration with Synergy, to analyze the deformity and plan the surgical steps.
Preoperative Preparation and Training Using Anatomical Models
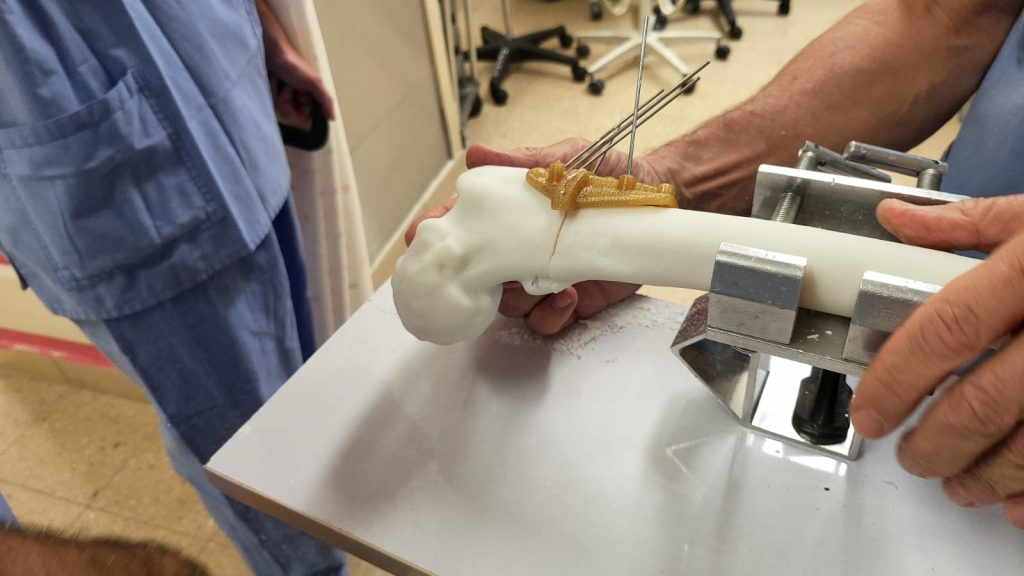
An anatomical model was created using Stratasys’ Digital Anatomy Printer (DAP) technology, mimicking natural bone structure. This model, printed on the J5 DAP printer, allowed for personalized surgical rehearsal and planning. Additionally, anatomical models printed using FDM technology with ABS material on an F170 printer facilitated pre- and post-surgical bone comparison, providing surgeons with an additional verification that the surgical plan was precise and feasible.
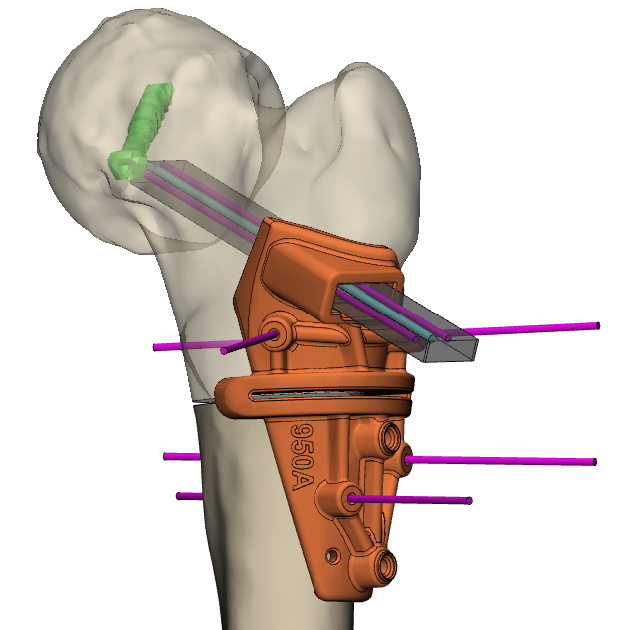
Development and Implementation of Customized Patient-Specific Instrumentation (PSI)
-
An initial PSI prototype was developed using ABS material and, after preliminary validation, was printed on a Fortus 450 printer using Ultem 1010 material.
-
The PSI enabled surgeons to verify the surgical plan with existing instruments, ensuring compatibility with the procedure and allowing for necessary adjustments.
-
The ability to preselect instruments and confirm procedural accuracy improved surgical preparation, reduced risks, and enhanced teamwork in the operating room.
Surgical Procedure and Integration of Personalized Planning
In this procedure, advanced 3D printing technologies were employed to enhance precision, efficiency, and clinical outcomes. The preoperative surgical planning and use of PSI significantly contributed to the success of the operation, streamlining the procedure and reducing surgical time by approximately two hours.
PSI Applications and Personalized Planning Benefits
-
Fixation with Kirschner Wires (KW) to ensure structural stability during the procedure.
-
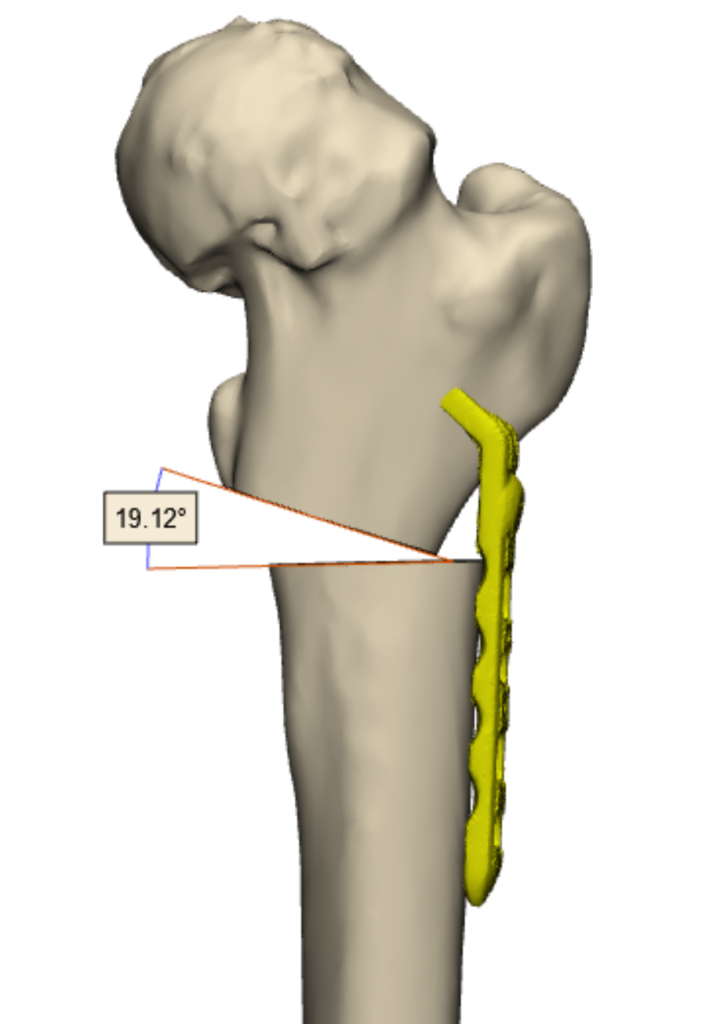
Bone cutting according to the pre-planned trajectory with high precision.
-
Drilling of pre-planned holes aligned with the CT-based simulation, perfectly matching the existing holes in the Ortho-Pediatrics Blade Plate.
-
Osteotome-assisted preparation of the femoral head for accurate insertion of the Blade Plate.
-
Preoperative verification of tools and surgical steps – the PSI allowed surgeons to assess instrument suitability and make necessary adjustments before surgery.
Key Advantages of Surgical Planning and PSI Utilization
✔ Enhanced Surgical Precision – Improved implant fit, reduced errors, and better procedural predictability. ✔ Reduced Complications – Lower risk of infections, nonunion, and recurrent fractures. ✔ Shorter Surgery Duration – More efficient procedures with reduced anesthesia time. ✔ Decreased Physical Strain on the Surgeon – Improved surgical workflow and reduced intraoperative uncertainty. ✔ Better Functional Outcomes – Reduced postoperative pain, improved quality of life, and precise anatomical restoration. ✔ DAP Material Advantages – Realistic bone simulation, precise preoperative planning, and enhanced surgical training.
Expert Testimonials
Dr. Danny Weigl, Head of the Pediatric Orthopedic Unit: “After using the anatomical model, I’d like to highlight several key points. The most educational stage is actually the planning phase, where we obtain precise data on the required correction in each of the three planes. This phase serves both as an analysis of the problem and as a means to develop a solution. The preparation of the internal fixation device on the corrected model, along with the use of the cutting jig, enables the most precise execution of the plan and saves significant surgical time. Performing osteotomies on the DAP model using the cutting jig helps identify potential issues, allowing for modifications in advance. Practicing the surgery on the model reveals anticipated intraoperative challenges, ensuring the surgeon enters the procedure well-prepared, minimizing errors and the need for repeated actions. The surgery’s efficiency and duration significantly improve.”
Dr. Paz Kedem, Pediatric Orthopedic Surgeon: “The 3D reconstructions allowed us to plan the surgery so that the final result mirrored the contralateral healthy hip. During the jig design process, we encountered multiple technical challenges that the medical designer from Synergy identified and resolved. Once completed, we performed a ‘dry run’ surgery using the actual surgical instruments, printed jigs, and the patient’s DAP bone model – a critical step that revealed unforeseen issues. The material used in the model is particularly noteworthy, as it closely mimics real bone and is much easier to work with compared to fragile and brittle saw bones. During the actual surgery, everything proceeded as planned, yielding results identical to the preoperative plan. In my opinion, this process is irreplaceable in complex osteotomies requiring multi-plane correction.”
Mr Michael Librus, CEO and founder of Synergy3DMed: “I wouldn’t allow a surgeon performing this procedure for the first time to operate without training on a DAP model.”
Conclusion and Future Outlook
The successful reconstruction of the femoral head was achieved through the integration of advanced 3D planning and personalized PSI. The use of PSI enabled maximum precision, reduced errors, and significantly improved surgical workflow.
Looking ahead, further advancements in 3D technologies and PSI are expected to enhance surgical accuracy and allow for even greater patient-specific customization. The next generation of medical printing materials, particularly Digital Anatomy Printer (DAP) technology, is anticipated to improve realism in simulating tissues and bones. Already, this material can replicate not only bony structures but also blood vessels, soft tissues, and cartilage, allowing for near-realistic surgical simulations and training.
Future developments in DAP technology are expected to provide even more advanced biomechanical properties, such as tissue response to pressure, natural flexibility, and adaptation to various cutting and drilling techniques. Additionally, the integration of artificial intelligence in planning processes may streamline model creation and offer intelligent analyses of bone structures and necessary corrections. Expanding the use of advanced anatomical models and PSI will help reduce risks, shorten surgical durations, and significantly improve clinical outcomes while fostering collaboration between medical institutions and the 3D printing industry.